Neuromuscular Electrical Stimulation for Treatment of Foot Drop
Main Article: "Functional electrical stimulation of walking: Function, exercise and rehabilitation" - T.A. Thrasher and M.R. Popovic
Neuromuscular electrical stimulation is a form of therapy for the treatment of the disorder known as foot drop. Foot drop is a syndrome which occurs when some damage occurs to the nervous system that prevents the toe or ankle dorsiflexors from operating at a high enough level to effectively prevent the toe from clearing the ground during the swing phase of walking gait. Foot drop is a problem that humans have been suffering from for as long a time as neurological disorders have existed. Over time, it has strongly adverse effects on the legs.
In the past, many mechanical orthotics have been used to help prevent foot drop. These range from immobile orthotics to dynamic hinged orthotics depending on each individual patient’s specific needs. Over time, mechanical orthotics have been gradually replaced by improved electrical stimulation orthotics. These work not by mechanically supporting the leg, but by providing innervating electrical stimulation to the nerves in the leg which allow the patient to clear the ground during the swing phase of gait. Neuromuscular electrical stimulation based orthotics help foot drop patients live more carefree, fulfilling lives.
Contents
Neuromuscular Electrical Stimulation
Emerging and Future Research Trends
Background
Walking and the Nervous System
Walking is a complex rhythmic locomotion function that requires several different parts of the brain and spine, and portions of the nervous system [12]. When a human decides to walk, a neural network in the spinal cord called the central pattern generator (or CPG) is triggered. The CPG innervates the proper somatic motor neurons to trigger the walking motion. [59] The CPG for walking is located in the spinal cord with higher center input and integration from and between the brain stem, cerebellum, thalamus and cerebral cortex. Once the signal has traveled those higher pathways, the signals go back down to the cortico-spinal cord. From here, they travel through somatic motor neurons to innervate the legs.[12]
The main conduit of the somatic system through and in the leg is through the peroneal nerve. The peroneal nerve is the primary nerve innervating the lower leg from the central nervous system (CNS), and carries motor commands from the brain to their destination. Along the way, the peroneal nerve branches many times to subsidiary nerves that innervate the surrounding musculature as the peroneal nerve continues toward the foot. The divisions begin just after the knee. The primary peroneal nerve continues down to the ankle where it splits into the medial cutaneous branch and the lateral cutaneous branch.[11]

The peroneal nerve and its branches innervate the surrounding tissues. [19]

Anatomical deformation vs. stance phase in a normal gait. [54]
Foot Drop
Foot drop is damage to the lower leg that can be described as extreme weakness of the ankle and toe dorsiflexors. This weakness results in the inability of the sufferer to angle their feet sufficiently high enough in order for their toes to clear the ground when they are walking. This forces a compensation which usually manifests itself in an irregular steppage gait. Most commonly, sufferers tend to increase the degree to which they swing their hips and raise their knees. [47] In so doing, the patient is able to raise the foot high enough to prevent the toe from dragging, and prevent it from hitting or slapping the ground. Other abnormal gaits can be developed, including a wide outward leg swing to avoid lifting the thigh excessively. [46] These abnormal gaits enable the sufferers’ toes to clear the ground during the swing phase of motion, but result in several negative consequences over time. Firstly, the heel winds up striking the ground, absorbing a force that is greater than body weight. This force also affects the knee negatively. This can result in severe damage to the heel and knee over time which can result in an equinovarus deformity, where the feet become increasingly rotated outwards and the knees bend outwards. [11] These gait alterations can be seen in the video below of foot drop in a pediatric patient.
Pediatric Hemipareisis - The right side of the body appears to be flaccid, and normal gait is disrupted by foot drop. [9]
Causes of Foot Drop
The phrase foot drop describes a potentially complex problem. Foot drop can be caused by mononeuropathies of the peroneal or sciatic nerves or other neurological problems such as lumbosacral plexopathy, compartment syndromes, lumbar radiculopathy, motor neuron disease, autoimmune diseases in the CNS and stroke. Peroneal neuropathy, or damage to the peroneal nerves can result from several sources, including peroneal, dorsiflexor or peripheral nerve injury, stroke, drug toxicity or diabetes. [11]
When these types of nerve damage occur, the muscles in the leg that provide stability and support for the foot during normal walking are unable to give the foot proper clearance from the ground. Additionally, the angle of the foot's strike against the ground can result in a normal force vector from the ground to the heel that exceeds a typical force on the heel. This can result in further injury, though lengthening of the anterior tibalis often absorbs the strike of the heel. [19]
Extensive physical models of this condition have been constructed, and involve complex force analysis. Understanding the physics driving the condition will allow more effective treatment of not only its symptoms, but its causes, as well. Generally, there is no "easy way" to treat foot drop; the only effective treatment is to deal with the underlying cause [28].
Peroneal Neuropathy
Damage to the peroneal nerve is most frequently caused by traumatic physical damage to the nerve itself. This can occur when the hip is impacted severely, such as in the case of an automobile accident or as a result of complications during hip replacement surgery.
Neuropathy is a term used to describe the dysfunction of the peripheral nervous system. It is generally considered analagous to peripheral neuropathy, defined as abnormal functioning of motor, sensory, and autonomic neurons [25]. Peroneal neuropathy in specific relates to dysfunction in the peroneal nerve, resulting in a condition known as foot drop.
While there are many potential causes of peroneal neuropathy, and the official definition does not identify a cause [26], chronic peroneal neuropathy can be caused by long-term bed rest, knee hyperflexion, general peripheral neuropathy, long-term leg crossing, prolonged pressure on the peroneal nerve, and even excessive physical conditioning, as is often seen in ballet dancers [27].

From the Columbia University Medical Center: "Magnified intraoperative photograph showing the common peroneal nerve (C) and its branches after decompression across the fibular head (F). Visible branches include the articular branch (1), deep division (2), superficial division (3), and branch to the peroneus longus muscle (4)."[70]
Lumbosacral Plexopathy
Lumbosacral plexopathy is a type of peripheral neuropathy in which nerve plexi in the lumbosacral regions of the spine are damaged. These regions of the spinal cord innervate and carry senses to and from the brain and the lower body.[60] This defect can be caused by immune vasculopathy, hemorrhage, physical trauma, ischemia, and complications from Intra-Arterial injection and Obstetric-Gynecological complications.[61]
Lumbar Rediculopathy
Lumbar rediculopathy is a similar neuropathy to plexopathy except that it afflicts roots in the lumbar region of the spine, which are part of the nervous system that innervates the lower body. Rediculopathy can have a variety of effects beyond decreased neuronal stimulation including intense pain, and is caused by intervertebral disc herniation.[62]

Image of the lumbar of a 46 year old male with lumbar radiculopathy, which was thought to be related to a disc herniation.[71]
Compartment Syndrome
Compartment syndrome occurs when an inflammation in a tightly enclosed area in the body such as an intervetebral region or joint causes an adjacent nerve to become compressed, leading to a variety of negative effects, including but not limited to, the impairment of that nerve.[63]
Amyotrophic Lateral Sclerosis
Motor neuron diseases such as amyotropic lateral sclerosis (ALS) affect the entire nervous system by attacking and destroying somatic motor cells. These neurons innervate all muscles that contribute to voluntary muscle movement. Though ALS eventually causes complete cessation to all voluntary motion, in the beginning and intermediate stages it causes weakness and atrophy in any or all muscles that are voluntarily controlled, leading to a variety of symptoms which can include foot drop.[64]
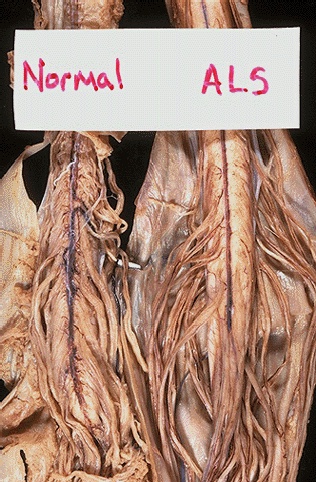
A comparison between the inside of a normal spinal cord and a spinal cord from an ALS patient.[69]
Stroke
Stroke is one of the leading causes of foot drop.[11] A stroke occurs when a blood vessel in the brain bursts, causing a region of the brain that is fed by that vessel to become starved of oxygen as well as hemorrhaging blood into the surrounding area of the brain.[65] Strokes can have a huge variety of negative effects on the central nervous system, including paralysis and numbness to either side of the body which can result in foot drop.[66]
Multiple Sclerosis
Foot drop can often manifest as a result of poor neural signaling resulting from multiple sclerosis (MS). MS is an autoimmune disease in which the axons of nerves in the central nervous system become demyelinated. [67] Nerves communicate by using action potentials to propagate electrical signals. This propagation occurs along shafts called axons, which are coated in an insulating material known as myelin. In MS, the myelin sheaths around the axons are attacked by the host’s immune system, resulting in weakened electrical signaling between neurons. This damage is especially prevalent in the white matter of the brain and in the spinal cord, which are mainly composed of myelin. [68] Due to this damage and the corresponding weakened signaling, signals that transverse the peroneal nerve are often too weak to allow for a normal gait, potentially resulting in foot drop.

Demyelinated nerves as a result of multiple sclerosis.[69]
Historical Treatments
Historically, the impairment of gait called for treatment with an ankle-foot orthosis (AFO). An AFO is a brace that is strapped around the ankle that increases area and force of the contact with the ground. In subjects with paretic ankle dorsiflexors, an AFO prevents foot drop during the swing phase of gait and helps to control foot placement after heel strike [51]. These braces were orginally built with metal and leather straps but since the late 1960's have been specifically molded to patients via the use of plastics. As of the 1990's carbon fiber and kevlar AFO's have been developed which combine great strength with low weight for an extremely effective AFO [29] . There are several types of AFO's that are currently available for clinical use including short leg fixed, dorsiflexion assist, solid ankle, full leg posterior leaf spring, and energy return AFO's. A less common AFO that is still worth mentioning is the Electro Hydraulic Ankle Foot Orthosis. Each of these ankle-foot orthotics is discussed briefly below.
The Short Leg Ankle Foot Orthosis

Image 2: Short Leg AFO [45]
The Short Leg AFO provides assitance with footdrop by limiting the angle of the foot to the leg at a constant ninety degrees. The Short Leg Ankle Foot Orthosis also limits movement inwardly to prevent the associated adaptation of gait that many patients with footdrop develop. This ankle foot orthosis is light and short allowing it to be worn inside the shoe to hide the AFO.[45]
Dorsiflexion Assist Ankle Foot Orthosis
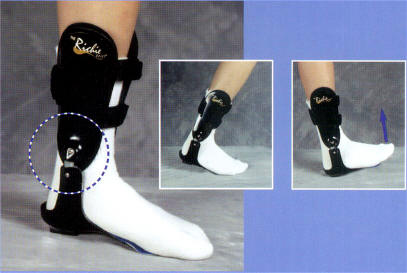
Dorsiflexion Assist AFO [45]

Becker Progressive AFO [30]
This Ankle Foot Orthosis combines the simplicity of the short leg AFO with a hinge at the ankle that allows for dorsiflexion. This AFO is widely used in cases of moderate footdrop, as the simple hinge will work to increase dorsiflexion enough to restore normal gait that had been disrupted [45].
Plantarflexion Stop Ankle Foot Orthosis

Plantarflexion Stop AFO [45]
This AFO is rigid at the base as to prevent cases of plantarflexion. Plantarflexion is less commonly associated with cases of footdrop, but nonetheless can develop. A hinge is built in to assist with dorsiflexion as in the Dorsiflexion assist AFO. The Plantarflexion Stop Ankle Foot Orthosis is bulkier than the two previous models as the entire base of the foot must be held in place to completely negate and plantarflexion [45].
Electro Hydraulic Ankle Foot Orthosis

Electro Hydraulic Ankle Foot Orthosis [48]
The Electro Hydraulic AFO is an extremely hefty system that can completely take over the responsibility of the central nervous system in control of gait. These are used after severe nerve damage if the patient has a total inability to innervate a walking motion. In use of these bulky orthesis, it is hoped that the person will be able to improve to a point where a more independent and light ortosis can be used. [48]
Solid Ankle Foot Orthosis

Solid AFO [45]
The Solid Ankle Foot Orthosis is the most basic form of an ankle foot orthosis. This AFO simply wraps around the calf, ankle, and foot and holds them in place disrupting both dorsiflexion and plantarflexion. The Solid AFO is useful in cases of severe footdrop, as the abnormal adaptation to gait is controlled entirely. This does not however restore normal gait as no true doriflexion or plantarflexion take place.[45]
Posterior Leaf Spring Ankle Foot Orthosis

PLS AFO [49]
The Posterior Leaf Spring Ankle Foot Orthosis wraps around the calf, ankle, and foot similarily to the Solid AFO. The main difference is that the foot is not held there as there are no straps and the plactics used are generally thinner and lighter. This provides for an ability to stimulate dorsiflexion of the ankle as the foot is not entierly inhibited. The thin plastics that are used make this AFO very light and it can be hidden inside of a sock. [49]
Energy Return Ankle Foot Orthosis

Energy Return Ankle Foot Orthosis [45]
The Energy Return AFO combines the classic properties of most AFO with the dynamic energy storing properties of carbon-fiber. These AFO's are able to retain the force of impact of the initial step and use it to assist in the dorsiflexion of the ankle. These devices are more modern as carbon fiber is being recently introduced into AFO technology by companies such as Royce Medical, which markets the Ossur [50] device. The advantages that are inherit in the use of carbon fiber also include the light weight of the material as well as the strength that it provides.
Though the AFO has been the standard treatment for foot drop for several years, it has both advantages and disadvantages when being used. Some studies have shown a benefit to the use of AFO’s that develops from the fact that form follows function. As additional weight is placed on the ankle during walking, more mineral deposition is allowed in the ankle, allowing it to grow stronger than the standard ankle with hemiparesis [29]. However, the use of an AFO also diminishes the possibility for active plantarflexion, inversion, and eversion [51]. Some AFO restrict these movements completely while others only limit the degree to which these activities can be performed. Because of these restrictions, gait analysis of subjects using an AFO shows that the gait pattern has several alterations in the duration of stance phase as well as the range of motion of the hip and knee. These alterations are not as severe as those that exist without the orthotic, but are still undesirable [52].
In 1961 WT Liberson H.j. Holmquest, D Scot, and M. Dow, published an article titled "Functional electrotherapy: stimulation of the peroneal nerve synchronized with the swing phase of the gait of hemiplegic patients, which is the first use of electrical stimulation to assist in foot drop" [41] . This breakthrough has provided us with the basis of all current treatment of foot-drop. The study showed by applying pulses for twenty micro seconds thirty times a second to the peroneal nerve through an electrode that the gait was significantly improved and they already showed signs of carry-over improvement. More on the development of neuromuscular electrical stimulation will be covered in the following section.
Neuromuscular Electrical Stimulation
How does it work?
Nerve Stimulation
Neuromuscular electrical stimulation(NMES), also known as functional electrical stimulation (FES), can be used as both a therapeutic treatment and as an aid for daily living. In both cases, the technology works by using low levels of electrical current to stimulate nerves in the affected extremity. In the specific case of foot drop, the nerve stimulated is the peroneal nerve, which runs along the outside of the lower leg below the knee. The peroneal nerve innervates the muscles which control foot lift and causes dorsiflexion, or lifting of the toes, when stimulated [7]. The stimulating electrodes can be on the surface or implanted, depending on patient and doctor preference. The obvious advantage to surface electrodes versus implanted electrodes is that surface electrode devices are much easier to remove should the need arise. However, this easy removal means that each of the surface electrodes must be properly placed again each time the device is worn as opposed to implanted electrodes which only need placement once. Implanted electrodes and sensors also allow for a much more cosmetically pleasing effect for the patient when compared to a surface system that is visible when worn. Comparative studies also show more subtle but noticeable differences between surface and implanted NMES electrodes. A comparative study by Pierce et al. showed that implanted electrical stimulation devices produced a greater degree of dorsiflexion than surface electrical stimulation when the same degree of stimulation was applied [14]. Another comparative study by Chae et al. has shown that patient discomfort levels are significantly lower when using implanted electrodes as opposed to surface electrodes [15]. Despite these differences, there has been no overall definitive difference found to prove one method of stimulation to be drastically better than the other and the treatment method used is still mainly based on patient needs and preference. The principle aim of implantable systems is to establish an orthotic effect rather than producing motor relearning effects. When motor relearning is the main goal, surface stimulators are more indicated [39].
The number of stimulation channels, or the number of individually programmable electrode pairs, used for electrical stimulation can also vary based on patient needs and preference. The most common NMES devices for foot drop consist of single-channel and dual-channel devices. Single channel devices are simplest to use, requiring little programming and minimal electrode placement, however they do not allow a high level of selectivity over which muscle groups and nerves are recruited. Because of this problem, research has recently been pushing NMES devices towards a dual-channel approach [34]. In the body, the peroneal nerve splits into two branches, one which lifts the foot and turns it inwards and one which turns the foot outwards. In normal walking, a combination of these movements is used. Thus, to achieve ideal gait pattern, it is theorized that two channels should be used to selectively stimulate each nerve branch at the appropriate time [33]. The STIMuSTEP system is one commercially available system that uses dual channel electrodes in this way. A diagram of the device can be seen below.

The STIMuSTEP Foot Drop Stimulator [44]
In the figure above, it should be noted that the device is an implanted dual-channel device where A is the external control unit, B is the leg strap, C is the heel switch, D is the implant receiver, E is the connecting cables, and F is the dual channel electrodes [44]. To date, both single-channel and dual-channel NMES devices have been successful in correcting foot drop and no definitive evidence has been presented to sway the field towards either choice.
Activation Switches and Sensors
Neuromuscular electrical stimulation devices require a type of activation switch or sensor to relay information about a patient's body position and gait to the device. With the information relayed from the sensor, the NMES device can choose the appropriate time at which to stimulate the peroneal nerve to provide the smoothest gait possible. Several types of switches and sensors can be used depending on the manufacturer and the specific device. The most common types of switches and sensors found in today's electrical stimulation devices are the heel switch and the tile sensor accelerometer.
The heel switch was a part of the original Liberson NMES for foot drop and is still in use today in devices like the STIMuSTEP. Liberson's design for the heel switch was very simple. A small switch was placed under the heel of the patient, usually within their shoe, and wired to the NMES device. When the foot was lifted at toe-off, the heel of the foot did not exert pressure and the heel switch was "open", allowing the peroneal nerve to be stimulated and lifting the toes. When the foot set down on the floor at heel strike, pressure was applied and the heel switch was "closed", cutting off stimulation to the nerve and allowing the foot to rest properly on the floor [41]. Since Liberson's original heel switch, several different modifications have been made by researchers and companies, such as heel switches filled with air (stimulation triggered by air pressure differences) and the incorporation of potentiometers into the switch to adjust the ramping rate (rate of change of the stimulus) at toe-off and heel-touch [20]. However, the overall design and triggering pattern has remained the same. The figure below shows a simplified diagram of the stance phase of gate for a better visual reference on the mechanics of the heel switch.

The Stance Phase of the Human Gait Cycle [43]
Two very important innovations regarding the heel switch system are worth mentioning. First was the addition of a "toe switch" to the heel switch system. This second switch is placed under the toes and acts as a control, preventing activation of the NMES device unless pressure is applied to it during the toe-off phase of gait. This prevents undesired stimulation if the patient lifted their heel to rest [42]. The toe switch is sometimes, but not always, used in today's NMES devices. The second innovation was the wireless switch which allowed patients to wear an FES device without having wires running up their legs [35]. However, the heel switch is still considered to be at a slight disadvantage because of the constant abuse it sustains from the daily ritual of being stepped on and the limited amount of information it is capable of gathering [20].
The tilt sensor accelerometer is a more recent innovation in the NMES world. The tilt sensor, which is an accelerometer that responds to tilt with respect to gravity [23], was just recently incorporated into the commercially released WalkAide system. It overcomes some of the disadvantages of the heel switch. The tilt sensor is attached just below the knee and works in a way that is very similar to the heel switch, but it detects tilt of the leg rather than pressure from the heel. When the leg is tilted back between heel-off and toe-off, the nerve is stimulated. When the leg tilts forward after hitting the ground, the stimulation turns off. The position of the tilt sensor allows for patients to use an NMES system in ways that they are unable to use a system with a heel switch, such as walking barefoot, and the ability to incorporate the system into one small device rather than several pieces makes tilt switch NMES devices easier for patients to use. The tilt sensor system also allows for an overall better cosmetic appearance with the same accuracy as a heel switch. When surveyed about their use of a tilt switch NMES, patients were overall very satisfied [21]. The WalkAide system can be seen in the figure below which shows the improved cosmetic appearance and ease of wearing.

The WalkAide System worn by a patient [24]
It should be noted that electrical stimulation is a treatment, not a cure, for foot drop. According to the National Multiple Sclerosis Society, "FES is not a cure but may restore or improve function in nerves that control specific muscles or muscle groups. FES can have therapeutic effects in some cases but it does not repair or regenerate the damaged spinal cord [7]". It should also be noted that though electrical stimulation is very effective in most cases of foot drop, it will not be effective in cases of foot drop due to specific motor neuron damage.
Assisted Walking Using Electrical Stimulation
Currently, many of the marketed electrical stimulation devices for treatment of foot drop are intended for use as functional orthotics for daily use to assist walking, such as the previously mentioned WalkAide system. As was discussed earlier, foot drop often results in an inability to clear the toes during walking and an abnormal gait pattern. The goal of NMES devices that act as functional orthotics is to assist or replace the AFO, which is often found to be stiff, uncomfortable, and awkward to use [36], in the treatment of this problem. Studies have presented several benefits to using NMES devices in treatment of foot drop as opposed to AFOs. These benefits include stimulation of circulation, increased walking distance, and better cosmetic acceptance [37] as well as a theoretical decreased need for compensation by the hip and knee during gait because of increased toe clearance [38]. Waters et al. provided some of the best evidence to support the use of NMES devices over the AFO, showing that an implanted electrical stimulation device could markedly increase average comfortable walking speed, step frequency and step length in patients who had previously been using an AFO. In some cases, the comfortable walking speed was increased by up to 36% [35].
Though many studies suggest that the use of NMES devices will completely replace the AFO in the future, some studies have found that better benefits may be obtained by combining these two treatments. A study by Kim et al. compared the use of NMES and hinged AFO alone to the use of the treatments combined. Though improvements in gait speed and distance walked were found when comparing each individual treatment to a baseline value of no treatment, the combination of NMES and AFO produced much greater improvements. The combination of treatments was found to increase walking speed up to 18% from a baseline value, nearly double the 10% increase granted by NMES alone [40]. Despite these promising results, there is still much research to be done on the benefits of NMES as compared to the benefits of the AFO and which treatment will be ideal for specific patient populations.
Theraputic Effects of Electrical Stimulation
Electrical stimulation in foot drop patients has been shown by some studies to be much more than simply a functional assistance. In many patients, electrical stimulation devices have been shown to have a therapeutic effect over periods of extended use. One recent study found that in patients with chronic hemiparesis, a severe weakening of one side of the body, continued use of an NMES device has been shown to not only improve gait velocity with further improvement as time progressed, but to also have effects on gait velocity carrying over to gait without NMES [10]. These results demonstrate the potential of NMES to act as a therapeutic agent and suggest that, with extended NMES therapy and use, patients can not only improve their mobility while using an NMES device, but they may also eventually be able to walk without NMES assistance. Another study performed recently examined and compared traditional therapy, NMES therapy, and a combination of traditional therapy and NMES therapy for treatment of foot drop. It was found that motor evoked potentials in the peroneal nerve of subjects that were treated with a combination therapy were increased by 66%, where traditional therapy and NMES therapy alone showed an increase of only 38% and 35% respectively. Since motor evoked potentials are a measure of the strength of connection between the brain and the muscle in innervates, these results imply that NMES may be a very effective tool for voluntary motor retraining, especially when combined with traditional therapy [13]. There is currently a lack of scientific studies on the specific therapeutic benefits of NMES, though electrical stimulation in addition to or in place of traditional therapies is currently a very active field of research with many advocates.
Emerging and Future Research Trends
One of the most visible and devastating disabilities in the world today is walking impairment due to hemiparesis. Much of the research has also been on the gait because studies have found out that this is the functional activity most valued by the patients [52]. The importance of performance and balance are consistently related to gait performance.
Home-Based Motor Imagery Training for Gait Rehabilitation
The recovery of walking ability is usually accomplished 12 weeks after a stroke. However, a gait impairment often remains that is mostly characterized by asymmetric pattern and slow speed. However, most of the equipment needed for home therapy is often not readily available for home use and is restricted to high end rehab centers. This situation is not ideal because the patient will have to depend on external sources for transportation to rehabilitation centers. In some cases, it wouldn't even be possible for them to walk or visit the rehabilitation centers. Due to these limitations, motor imagery has emerged as a possible solution. Motor imagery increases the brain activity in the neuronal cortical networks. The stimulation of neuronal cortical networks helps in learning and relearning of motor tasks. Since it is low cost and low risk motor rehabilitation, it will is a usually considered to be a very effective treatment. Various brain imaging studies has suggested that the same sizable area is activated during actual performance and during mental rehearsal of the same tasks. The treatment is most effective when treated early in the rehabilitaiton phase. In this home-based procedure, specified minutes of supervised imagery gait training is given in the patient's home 3 days a week for 6 weeks. It affected lower limb and task-specific gait training [16].
Research has shown that when walking ability was evaluated by kinematics and functional scales twice before the intervention, 3 and 6 weeks after the intervention, and at the 3-week follow-up period, significant improvement was seen. In this training, the first 4 weeks is focused on the enhancement of imagery training of push-off performance by the paretic leg and on prolongation of the loading phase of that leg. During the last 2 weeks, patients were directed to increase their imagined speed and symmetry of walking. Various walking tasks were involved by using visual imagery in which the patients viewed themselves from perspective of an external observer. Kinesthetic imagery was also used which allowed the participants to experience the same sensation of bodily functions in an actual situation. The natural cadence was maintained using chronometric measurement and syncing the walk using metronome. After the tempo was maintained the metronome is turned off and patient continues to walk in the same pace [16].
"Walk-Mate" System
Motor paralysis and motor impairment are the chief causes behind gait impairment. There are two main approaches in gait treatment of this type, one using the "Walk-Mate". The firs approach involves gait compensation by using techniques to replace the impairment. This replacement is done using supporting devices such as wheel chairs and walking sticks. Other replacements came about with the advent of bioprosthesis and various other techniques such as load-controlled gait assistance devices, power-assistive gait support machines, and powered suits. All these techniques stimulate elements of lower body motion (range of joint motion and physical strength) using actuators. However, the patient will is required to function under the limitation imposed by the supporting devices. Also, continuous usage may lead to slow decline in normal gait pattern. The second approach is restoration of neurophysiological functions. This can be done using devices that help the patient to improve their gait capability by training and exercise with the help of machines and trainers. Walk-Mate gait system is one device that works by providing assistance in locomotion as well as gait rehabilitation training. A model gait rhythm is generated in response to patient's real-time locomotion. It is presented as auditory stimuli supporting locomotion by stabilizing the rhythm of foot contacts [17].

Walk-Mate System [17].
Functional Electrical Stimulation Techniques
The use of electrical stimulation was first demonstrated by Liberson in 1961. By applying continuous FES on quadriceps and gluteus maximus muscles of a patient with complete Spinal Cord Injury, he was able to show movement in paraplegic patients. This movement allowed full extension of lower limbs, and enabled some form of gait similar to walking gait with braces. Several devices based on this technology are out in market, majority of them still waiting for Food and Drug Administration (FDA) approval. Some of them are discussed below.
Parastep-I® system
The Parastep-I is based on Kralj's technique. According to Kralj's technique, four channels of stimulation should be used. Skin electrodes are placed over the quadriceps muscles and peroneal nerves bilaterally. The user controls the FES device with two pushbuttons attached to the left and right handles of a walking frame which can be either canes or crutches. When the FES device is activated, both quadriceps muscles are stimulated. The left button initiates swing phase in the left leg by briefly stopping stimulation of the left quadriceps and stimulating the left peroneal nerve. This stimulation is applied suddenly so as to trigger the flexor withdrawal reflex, resulting in simultaneous hip and knee flexion as well as dorsiflexion. After a fixed period of time, peroneal nerve stimulation is stopped and quadriceps stimulation is resumed. Similarly, the right button initiates swing phase in the right leg. Kralj et al. successfully applied this system to several dozen subjects with SCI. The full device has now received FDA approval. It is used by patients with paraplegia (both complete and incomplete) every time they wish to walk. It includes a two-wheeled walker and an ankle-foot orthosis to bolster ankle stiffness. The Parastep-I® is commercially available, and over 600 people have used it successfully. A major disadvantage of systems that use the Kralj technique is that they rely on the flexor withdraw reflex, which is variable and subject to habituation [18].

Parastep-I® system [57].
Praxis24 system
The Praxis24 is a fully-implanted system that is convenient and is able to stimulate deep lying muscles such as hip flexors. It has a greater muscle selectively and can provide bladder voiding. However, it can only provide swing-through gait pattern. It has been approved by FDA but records indicate that this system has been implanted on very small number of patients [18].
Foot Drop Stimulators
These are special class of FES which is more specific to foot drop, a problem which is caused by lack of dorsiflexion due to weakness of the tibialis anterior muscle. Most FDS devices are simple, single-channel systems that are intended for everyday use, such as Liberson's invention in 1961. They are used mostly by people with hemiplegia due to stroke, but are also used bilaterally by some people with paraplegia. There are several FDS available in market. The first FDS devices were MikroFES (Josef-Stefan Institute, Ljubljana, Slovenia) and the Odstock Dropped Foot Stimulator. Research has shown that these systems significantly increase walking speed and efficiency when used but they have a disadvantage in that they use surface electrodes. The first fully implantable FDS was developed by Rancho Los Amigos Medical Centre and Medtronic, Inc. The surgically implanted components consisted of a radio-frequency (RF) receiver, pulse train generator, and one bipolar electrode implanted adjacent to the peroneal nerve. The power was delivered by an external unit worn on the belt via the RF coil and received input commands from a wireless foot switch. Although there were problems with electrode migration and infection, the device was considered successful. Since then, more reliable and easier to implant systems have been devised, such as the Neurostep system and the ActiGait, but they are not yet commercially available. ActiGait uses biofeedback input from an implanted cuff electrode around the sural nerve (nerve innervating the skin sensors on the sole of the foot). This system does not require external sensors [18]. ActiGait is based on implanted stimulator which activates the foot lift by stimulating the peroneal nerve above the knee which results in activation of lower leg muscles. This creates a dorsiflexor reflex which lifts the foot. The stimulating electrode is located under the skin just above the knee while the stimulator is located under the skin on the thigh. The surgical procedure is very short. The stimulator is controlled by an external control unit which can be carried in the belt. The energy is transmitted from the control unit and signal is transmitted to the stimulator via an antenna place on the skin over the stimulator. The stimulation is activated by wireless heel switch located in the shoe [56].

Acti-Gait System [58].
Neurostep is a "neurostimulation investigational medical device" which is surgically implanted inside the leg of a patient. The electrodes that are attached to the peripheral nerves sense the heel position and stimulate the proper muscles to lift the foot during normal walking. Since the system is surgically connected directly to the targeted nerves, a “closed loop” is established that provides greater mobility and more natural movements. It has a battery operated Control Unit which is always on. This allows it to sense key physical events, interpret them and stimulate specific muscles of the ankle. For example it helps in flexing the foot at the right time so the toes no longer drag across the ground [53].

Accelerometers as Sensors
The accelerometer, which began its development in the NMES world around 1986, almost thirty years after Liberson's heel switch, is still a hot topic in current research. The accelerometer detects the subtle differences in acceleration during gait and uses these differences to trigger nerve stimulation. Though the tilt switch is one use of an accerometer in current use, many scientists believe that accelerometers can be used in a different way to smooth gate even further when using a NMES device. A recent study by Shimada et al. found that it was possible to use a single accelerometer in cooperation with a program called Neural Network to accurately study and record the gait cycles of normal patients and those with foot drop. They proposed a possible combination of this technology with NMES electrodes to improve cosmetic appearance of NMES devices further, improve the ease of applying sensors, and overcome several limitations of foot switches [22].
References
[1] R. Chin et al., "A pneumatic power harvesting ankle-foot orthosis to prevent foot drop," Journal of Neuroengineering Rehabilitation, vol. 6, no. 19, June 2009. [Online]. Available: PubMed, http://www.pubmedcentral.nih.gov. [Accessed July 12, 2009].
[2] Cruz, T. H. and Y. Y. Dahaher, "Impact of ankle-foot-orthosis on frontal plane behaviors post-stroke," Gait & Posture, June 2009. [Online]. Available: ScienceDirect, http://www.sciencedirect.com/. [Accessed July 12, 2009].
[3] M.R. Mulvey, H.J. Fawkner, H. Radford and M.I. Johnson, "The use of transcutaneous electrical nerve stimulation (TENS) to aid perceptual embodiment of prosthetic limbs," Medical Hypotheses, vol. 72, issue 2, February 2009. Pages 140-142. Available: ScienceDirect, http://www.sciencedirect.com/. [Accessed July 12, 2009].
[4] Black, Carissa et al, "The Knee Nook. (Engineering Design and Communication Projects)," Topics in Stroke Rehabilitation vol. 15, no. 2, March-April 2008. [Online] Available: Academic OneFile, http://www.gale.cengage.com/. [Accessed July 12, 2009]
[5] Dobkin, B. H., "Strategies for stroke rehabilitation," The Lancet Neurology, vol. 3, no. 9, September 2004. [Online] Available: ScienceDirect, http://www.sciencedirect.com/. [Accessed July 12, 2009]
[6] Breen, Paul P. et al, "A programmable and portable NMES device for drop foot correction and blood flow assist applications," Medical Engineering & Physics, vol. 31, no. 3, April 2009. [Online] Available: ScienceDirect, http://www.sciencedirect.com/. [Accessed July 13, 2009]
[7] National Multiple Sclerosis Society, “Functional Electrical Stimulation”. [Online]. Available: http://www.nationalmssociety.org [Accessed: July 28, 2009].
[8] Prodanov, Dimiter. et al, "Functional Electrical Stimulation for Sensory and Motor Functions: Progress and Problems", Biomedical Reviews, vol. 14, 23-50, 2003. [Online] Available http://www.diagnosticarea.com/. [Accessed July 15, 2009]
[9] Kirtley, Chris "Case of the Week 20-1-2003" Very active 5 Year old boy with Right Spastic Hemiparesis. http://www.univie.ac.at/CGA/archives/20-1-03/ [Accessed: July 15, 2009]
[10] Laufer, Yocheved et al., "Gait in Individuals with Chronic Hemiparesis: One-Year Follow-up of the Effects of a Neuroprosthesis That Ameliorates Foot Drop," Journal of Neurologic Physical Therapy, vol. 33, no. 2, June 2009. [Online] Available: PubMed, http://pubmed.nih.gov [Accessed July 28, 2009]
[11] Pritchet, James W and Porembski, Margaret A, "Foot Drop", http://emedicine.medscape.com/article/1234607-overview, updated June 23rd, 2009, Accessed July 29th, 2009
[12] Silverthorn, Dee Unglaub, "Human Physiology: An Integrated Approach"
[13] Khaslavskaia, Svetlana et al., "Motor cortex excitability following repetitive electrical stimulation of the common peroneal nerve depends on the voluntary drive," Experimental Brain Research, vol. 162, no. 4, February 2005. [Online]. Available: SpringerLink, http://www.springerlink.com v. [Accessed July 29, 2009].
[14] Pierce, Samuel R. et al., "Comparison of Percutaneous and Surface Functional Electrical Stimulation During Gait in a Child with Hemiplegic Cerebral Palsy," American Journal of Physical Medicine & Rehabilitation, vol. 83, no. 10, October 2004. [Online]. Available: PubMed, http://pubmed.nih.gov. [Accessed July 29, 2009].
[15] Chae, John. et al., "Comparison of Discomfort Associated With Surface and Percutaneous Intramuscular Electrical Stimulation for Persons With Chronic Hemiplegia1," American Journal of Physical Medicine & Rehabilitation, vol. 77, no. 6, December 1998. [Online]. Available: PubMed, http://pubmed.nih.gov. [Accessed July 29, 2009].
[16] A. Dunsky, R. Dickstein, E. Marcovitz, S. Levy and J. Deutsch, "Home-Based Motor Imagery Training for Gait Rehabilitation of People With Chronic Poststroke Hemiparesis," Arch. Phys. Med. Rehabil., vol. 89, pp. 1580-1588, 8. 2008.
[17] T. Muto, B. Herzberger, J. Hermsdorfer, Y. Miyake and E. Poppel, "Interactive gait training device "walk-mate" for hemiparetic stroke rehabilitation," in 2007 IEEE/RSJ International Conference on Intelligent Robots and Systems, IROS 2007, October 29, 2007 - November 2, 2007, pp. 2268-2274.
[18] T. A. Thrasher and M. R. Popovic, "Functional electrical stimulation of walking: Function, exercise and rehabilitation," Annales De Réadaptation Et De Médecine Physique, vol. 51, pp. 452-460, 7. 2008.
[19] Pritchett, James, "Foot Drop" Deep peronela nerve, branches, and cutaneous innervation, http://img.medscape.com/pi/emed/ckb/orthopedic_surgery/1230552-1234607-65.jpg [Accessed July 22, 2009].
[20] Lyons, Gerard et al., "A Review of Portable FES-Based Neural Orthoses for the Correction of Drop Foot," IEEE Transactions on Neural Systems and Rehabilitaion Engineering, vol. 10, no. 4, December 2002. [Online] Available: IEEExplore, www.ieeexplore.ieee.org [Accessed August 18, 2009].
[21] Stein, Richard et al., "A Multicenter Trial of a Footdrop Stimulator Controlled by a Tilt Switch," Neurorehabilitation and Neural Repair, vol. 20, no. 3, 2006. [Online] Available: Academic OneFile, http://www.gale.cengage.com/ [Accessed August 18, 2009].
[22] Shimada, Yoichi et al., "Clinical Application of Acceleration Sensor to Detect the Swing Phase of Stroke Gait in Functional Electrical Stimulation," Tohoku Journal of Experimental Medicine, vol. 207, no. 3, November 2005. [Online] Available: Directory of Open Access Journals, www.jstage.jsp.go.jp [Accessed August 18, 2009].
[23] Stein, Richard et al., "Surface Electrical Stimulation for Foot Drop: Control Aspects and Walking Performance," Journal of Automatic Control, vol. 18, no. 2, 2008. [Online] Available: http://automatika.etf.bg.ac.yu/files/JAC/JAC2008_2/Rad%2005%20Dropfoot.pdf [Accessed August 19, 2009].
[24] Custom Orthotic Design Group Ltd., "Living with Foot Drop: Be More Active and Independent Wearing WalkAide." [Online] Available: http://www.customorthotic.ca/articles/walkaide.html [Accessed August 19, 2009].
[25] Dyck PJ (1982). "Current concepts in neurology. The causes, classification, and treatment of peripheral neuropathy". N. Engl. J. Med. 307 (5): 283–6. PMID 6283352, http://www.ncbi.nlm.nih.gov/pubmed/6283352 [Accessed August 19, 2009].
[26] Bogduk, Nikolai; Merskey, Harold (1994). Classification of chronic pain: descriptions of chronic pain syndromes and definitions of pain terms (2nd edition ed.). Seattle: IASP Press. pp. 212.
[27] Walter George Bradley (2004). "foot+drop" Neurology in clinical practice (4 ed.). Taylor & Francis. pp. 2545. ISBN 9997625889. page 453-454.
[28]Walid MS, Ajjan M, Patel N, T Guta: Cellulitis May Present As Foot Drop In A Diabetic Patient: The Internet Journal of Neurology. 2007; Volume 7, Number 1.
[29] O'Reilly Taylor et al "Effects of Ankle-Foot Orthoses for Children with Hemiplegia on Weight-Bearing and Functional Ability" Pediatric Physical Therapy Volume 21(3), Fall 2009, pp 225-234
[30] Becker Orthopedic "Progressive AFO Model 395" Copyright 2003 [Online] Available: http://www.beckerorthopedic.com/progressive_afo/progressive_afo.htm [Accessed August 19, 2009]
[31] "Peroneal Neuropathy" http://www.healthcentral.com/encyclopedia/408/212.html
[32] "Peripheral nerve injuries in the athelete" http://www.ncbi.nlm.nih.gov/pubmed/9421863
[33] Chevalerias O et al., “Inductive Powering for Biomedical Applications,” in 9th Annual Conference of the International FES Society, 2004
[34] Kenney, Laurence et al., “An Implantable Two Channel Drop Foot Stimulator: Initial Clinical Results,” Artificial Organs, vol. 26, no. 3, March 2002. [Online] Available: Wiley InterScience, www.interscience.wiley.com [Accessed August 23, 2009]
[35] Waters, RL., “Experimental Correction of Footdrop by Electrical Stimulation of the Peroneal Nerve,” The Journal of Bone and Joint Surgery, vol. 57, no. 8, 1975. [Online] Available: JB&JS, www.ejbjs.org [Accessed: August 23, 2009]
[36] Taylor PN et al., “Patients’ perceptions of the Odstock Dropped Foot Stimulator (ODFS),” Clinical Rehabilitation, vol. 13, no. 8, October 1999. [Online] Available: Sage Journals Online, www.cre.sagepub.com [Accessed: August 23, 2009]
[37] Buurke JH et al., “Ist der peronaeus-stimulator eine sinnvolle alternative zur unterschenkelorthese? Technik, anwendung und ergebnisse,” Med Orth Tech, vol. 110, 1990.
[38] Merletti R et al., “Clinical experience of electronic peroneal stimulators in 50 hemiparetic patients,” Scandinavian Journal of Rehabilitation Medicine, vol. 11, no. 3, 1979.
[39] Kottink, Anke et al., "The Orthotic Effect of Functional Electrical Stimulation on the Improvement of Walking in Stroke Patients with a Dropped Foot: A Systematic Review," Artificial Organs, vol. 26, no. 6, 2004. [Online] Available: Wiley InterScience, www.interscience.wiley.com [Accessed August 23, 2009]
[40] Kim, CM et al., “Effects of a simple functional electric system and/or a hinged ankle-foot orthosis on walking in persons with incomplete spinal cord injury,” Archives of Physical Medicine and Rehabilitation, vol. 85, no. 10, October 2004. [Online] Available: ScienceDirect, www.sciencedirect.com [Accessed August 23, 2009]
[41] W. T. Liberson et al., “Functional Electrotherapy in stimulation of the peroneal nerve synchronized with the swing phase of gait in hemiparetic patients,” Archives of Physical Medicine and Rehabilitation, vol. 42, February 1961.
[42] Strojnik P. et al., “Programmed six-channel electrical stimulator for complex stimulation of leg muscles during walking,” IEEE Transactions on Biomedical Engineering, vol. 26, no. 2, February 1979.
[43] “Lower Limb Biomechanics,” d-med.com, [Online] Available: http://www.d-med.com/aol/html/bmi.html [Accessed: August 23, 2009]
[44] "Finetech Dropped Foot System - STIMuSTEP," 2008, [Online] Available: http://finetech-medical.co.uk [Accessed: August 23, 2009]
[45] "Treating Dropfoot with Ankle Foot Orthosis" Foot and Ankle Center of Washington, 2005-2009, [Online] Available: http://www.footankle.com/drop-foot.htm [Accessed: August 23, 2009]
[46] "Foot Drop" Molson Medical Informatics Project, 1997-2000, [Online] Available: http://sprojects.mmi.mcgill.ca/gait/footdrop/intro.asp [Accessed: August 23, 2009]
[47] Alojz R. Kralj, Tadej Bajd. "Functional electrical stimulation : standing and walking after spinal cord injury" [vii], 198
[48] Noel et al. Journal of NeuroENgineering and Rehabillation 2009 6:16 doi:10.1186/1743-0003-6-16, [Online] Available: http://www.jneuroengrehab.com/ [Accessed: August 23, 2009]
[49] "AFO Posterior Leaf Spring" SkyMedical Inc. 2003-2009, [Online] Available: http://www.medcompare.com/matrix/1916/Ankle-Brace.html [Accessed: August 24, 2009]
[50] "Family of Ankle Foot Orthosis Products" -Ossur, Royce Medical , [Online] Available: http://www.ossur.com/lisalib/getfile.aspx?itemid=7460[Accessed: August 24, 2009]
[51] Geobers, Johanna et al., “Immediate and Long-Term Effects of Ankle-Foot Orthosis on Muscle Activity During Walking: A Randomized Study of Patients With Unilateral Foot Drop,” Archives of Physical Medicine and Rehabilitation, vol. 83, no. 2, February 2002 [Online] Available: ScienceDirect, www.sciencedirect.com [Accessed August 24, 2009]
[52] Lehmann JF et al., “Gait abnormalities in tibial nerve paralysis: a biomechanical study,” Archives of Physical Medicine and Rehabilitation, vol. 66, 1985.
[53] "Neurostep" Victhom Human Bionics. 2009, [Online] Available:[[http://www.medcompare.com/matrix/1916/Ankle-Brace.html|http://www.victhom.com/en/neurostimulation/neurostep.php]] [Accessed: August 24, 2009]
[54] Popovic, D.B and Stefanovic, F., "Control of the Lower Leg During Walking: A Versatile Model of the Foot," IEEE Transactions On Neural Systems and Rehabilitation Engineering, vol. 17, 2009.
[55] Roehrig S, Yates DA "Case report: effects of a new orthosis and physical therapy on gait in a subject with longstanding hemiplegia," J Geriatric Physical Therapy 2008; 31(1): 38-46
[56] "Acti-Gait" Neurodan. 2009, [Online] Available: http://neurodan.dk/actigait.asp , [Accessed: August 24, 2009]
[57] "The Parastep System" The Therapeutic Alliances. 2009, [Online] Available: http://www.musclepower.com/parastep.htm, [Accessed: August 24, 2009]
[58] "Acti-Gait" University of Southampton. 2009, [Online] Available: http://www.southampton.ac.uk/healthsciences/research/projects/MLC/ActiGait/index.html, [Accessed: August 24, 2009]
[59] Hooper, Scott L. “Central Pattern Generators.” 2001, Available online: http://crab-lab.zool.ohiou.edu/hooper/cpg.pdf [Accessed 23 August, 2009].
[60] National Library of Medicine. “Lumbosacral Plexus.” Available online: http://www.nlm.nih.gov/cgi/mesh/2009/MB_cgi?mode=&term=Lumbosacral+Plexus&field=entry [Accessed 23 August, 2009].
[61] “Nerve: Proximal Motor.” Available online: http://neuromuscular.wustl.edu/nanatomy/proxmot.html#lsplex [Accessed 23 August 2009].
[62] “Radiculopathies.” Available online: http://www.neuroanatomy.wisc.edu/SClinic/Radiculo/Radiculopathy.htm [Accessed 23 August 2009].
[63] User: Matt. “The Five P’s of Acute Compartment Syndrome.” 2005, Available online: http://www.compartmentsyndrome.net/ [Accessed 24 August 2009].
[64] National Institute of Neurological Disorders and Stroke. “Amyotrophic Lateral Sclerosis Fact Sheet.” 2008, Available online: http://www.ninds.nih.gov/disorders/amyotrophiclateralsclerosis/detail_amyotrophiclateralsclerosis.htm [Accessed 24 August 2009].
[65] National Institute of Neurological Disorders and Stroke. “NINDS Stroke Information Page.” 2009, Available online: http://www.ninds.nih.gov/disorders/stroke/stroke.htm [Accessed 24 August 2009].
[66] Mayo Clinic Staff. “Stroke Symptoms.” 2008, Available online: http://mayoclinic.com/health/stroke/DS00150/DSECTION=symptoms [Accessed 24 August 2009].
[67] Compston A, Coles A (April 2002). "Multiple sclerosis". Lancet 359 (9313): 1221–31.
[68] Charcot, J. Histologie de la sclerose en plaques. Gazette des hopitaux, Paris, 1868; 41: 554–555.
[69] Granovsky, D. “The Stem Cell Blog.” 2009, Available online: http://repairstemcell.files.wordpress.com/2009/02/ww5r308_big.jpg [Accessed 24 August 2009].
[70] Columbia University. “Peroneal Neuropathy.” 2008, Available online: http://www.cumc.columbia.edu/dept/peripheral-nerve/problems/pn_2.html [Accessed 24 August 2009].
[71] American Society of Spine Radiology. “January Case of the Month.” 2009, Available online: http://theassr.org/case-of-the-month/january-case-of-the-month-3/ [Accessed 24 August 2009].
[72] Mercer University School of Medicine. “ALS Pathology.” 2007, Available online: http://library.med.utah.edu/WebPath/jpeg5/CNS103.jpg [Accessed 24 August 2009].


No comments:
Post a Comment